Evolve: We Need Sustainability in the Pharmacy Profession
The pharmacy profession needs to evolve towards greater sustainability, encompassing environmental, economic, and social aspects.
Featured Blogger
August 17, 2025
04/09/20
“Adapt or die, the evolution of pharmacy”, you have come across this theme from the 2017 Zimbabwe pharmaceutical student’s association (ZPSA) conference in Kariba or at least something similar “Pharmacy needs to transform from product to service.” from the pharmacy times magazine.
Over the last few decades, a new movement has been espoused to preserve the relevancy of the pharmacy profession, by moving away from a (drug) product-oriented approach to a more clinical-based service in which the focus is the patient and the outcome. New manufacturing companies are being registered, innovations that are both cost-effective and efficient are being incorporated into daily drug manufacture, this will push the price of medication down hence pharmacists can no longer rely on product reimbursements or profits only.
The day is coming when product profits will not be able to pay for a pharmacist`s services, a day when non-pharmacists (pharmacy technicians and dispensing assistants) and robots will take over dispensing. The ongoing economic crisis in Zimbabwe has been mostly a curse but also a blessing in exposing the thin thread our profession is hanging on. Current trends have recorded low drug sales resulting in reduced salaries for pharmacists. One might argue a better economy and a more functional healthcare system would save the profession however what’s coming is inevitable and has been accelerated by the covid19 pandemic.
What can we do?
Pharmacists can push for “provider status” which can be translated to charging for consultations like other health professionals, thus, in the long run, generate scores of revenues. The details of how this can be implemented are still shaky amongst pharmacy leaders and the reader is free to ponder on how we could set up such a framework in Zimbabwe. This makes sense but it’s not that simple, and here is what we can do.
Patient-centred care
Longitudinal Patient Care aims to realize what the patient`s needs are and treatment is centred along with those needs. (Dyke, P et al., 2014) define longitudinal care as the “holistic, dynamic, and integrated plan that documents important disease prevention and treatment goals and plans. An LCP is patient-centred, reflecting a patient's values and preferences, and is dependent upon bidirectional communications.”
The use of Information technology/ electronic systems can then integrate the various elements of the LCP dynamically to generate an appropriate assessment for the provider and/or patient/family member thus providing information to identify and achieve the individual's health goals along the field of care. In the developed world payers are now migrating from fee-for-service reimbursement, though it is dependent on policymakers.
The “in” things in the realm of patient care are now chronic care management, outcomes-based recompense, and population care. Point-in-time meetings with patients are now regarded as not being sufficient enough to provide high-quality care. Forgive the writer for using statistics from the west but this can be attributed to the paucity of official statistics in our setting.
The centre for Medicare and Medicaid Services (CMS) announced that it is spending billions by changing the way the government of the United States reimburses professionals for physician care. The aim is to remove the exclusive focus on encounters and migrate toward contiguous, coordinated, longitudinal, and personalized health care distribution services. Trygstad, T in 2019 highlighted the need for such services to be transformed to pharmacists, he suggested that 83.2% of prescriptions filled by pharmacists in the United States are of patients with at least 2 chronic diseases, hence logically if we translate the figures to our setting one can argue that longitudinal care to pharmacist-provided services would improve the quality of services whilst creating a billable chain through dispensing and checkups.
This can be achieved by care plans that involve following ups which in time will lead to appointment-based models and contracts heavily associated with the clinical outcome as opposed to medication provision. Not only will pharmacists be able to expand their source of revenue but will also evolve to be better connected with patients giving a sense of fulfilment and improved mental health.
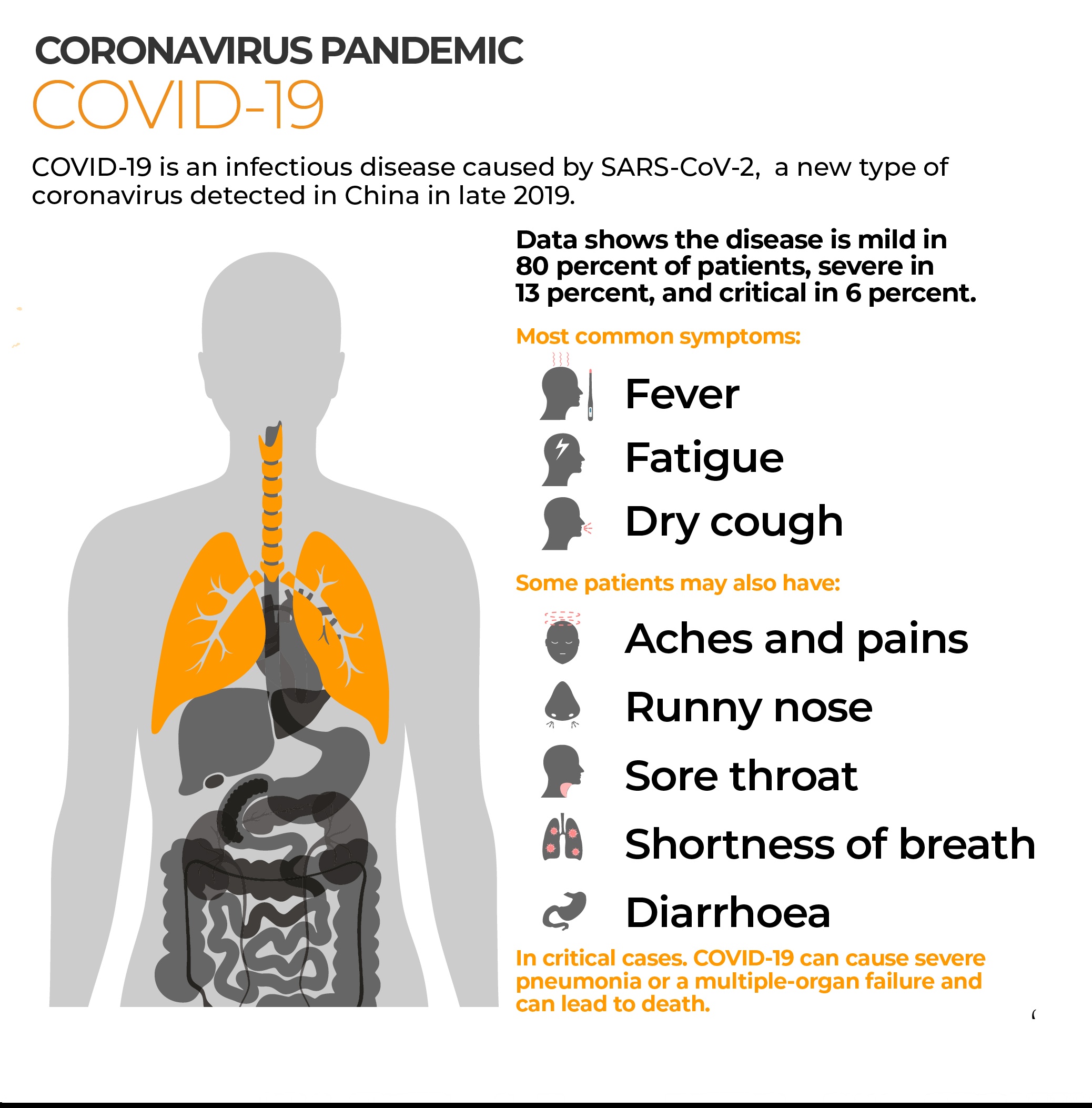
(See image attached on article)
Prescription Workflow, though strength is also our Biggest constraint
To my colleagues working in the retail sector, you provide patients with an accessible and dynamic environment filled with the scents of different medications and methylated spirit. This environment is welcoming and convenient however serves as a barrier to patient-level care delivery. There are always long queues and medications are dispensed in a rash.
A report from the Pharmacy times in 2019 shares the same view by giving an example of a diabetic patient. Mr Sibanda has not had his metformin filled in the last 4 months and is long due for a glycated haemoglobin (A1C) test. The current model of informatics and prescription processing does not address this problem/opportunity (depending who you are) nor does it provide a solution. Dear reader, are we doing enough for our profession as Zimbabweans?
Health Informatics should not be limited to hospitals and clinics
Daily patients are faced with numerous drugs and non-drug-related problems. There are many parameters to monitor if a patient is responding to treatment or not when following up and these include but are not limited to blood pressure, temperature, blood glucose level, treatment goals and treatment plans. We need information frameworks that address patient-level care to better coordinate care, and assure quality and most importantly billable. Dear reader, please refer to the Pharmacist eCare Plan Initiative (ecareplaninitiative.com) to be better understand the application of health informatics in pharmacy settings.
You can never replace a Pharmacist.
I do realize this is a bold claim which seems contradictory to the idea I`m pushing, however, a pharmacist is not defined by dispensing medication and you can close a pharmacy, even switch to online methods of prescription filling but professional judgement and patient to provider relationships are inimitable. If as Pharmacists we are to take a patient-centred care approach as a billed service our professional then will become untouchable. Longitudinal care planning is very much possible and it starts with you. Below is a dialogue of you and your patient a few years from now.
“Pharmacist counselling: How are you today, Tongai? This is your monthly amlodipine. Are you having any unusual troubles?
Patient at pickup: Actually, yes. I get dizzy when I stand up
Pharmacist: I see, you know what? Let's take your blood pressure.
Patient: Sure.
Pharmacist: It's 110 over 75. I`m okay with that. What time are you taking your amlodipine?
Patient: In the morning, and I feel dizzy in the afternoon
Pharmacist: Alright let`s move your dose to late afternoon and see how you feel next month
Pharmacist (next month): Hi, Tongai How are you feeling this month? We talked about moving the time you took your blood pressure medication....” (Trygstad T, 2019.)
This is an approach to pharmacy practice that is professionally fulfilling, lifelong and is already in place amongst other healthcare professionals.
References:
Azhar, S., Hassali, M. A., Ibrahim, M. I. M., Ahmad, M., Masood, I., & Shafie, A. A. (2009). The role of pharmacists in developing countries: the current scenario in Pakistan. Human Resources for Health, 7(1), 54.
Dykes, P. C., Samal, L., Donahue, M., Greenberg, J. O., Hurley, A. C., Hasan, O., ... & Bates, D. W. (2014). A patient-centred longitudinal care plan: vision versus reality. Journal of the American Medical Informatics Association, 21(6), 1082-1090.
Pharmacist eCare Plan Initiative. ecareplaninitiative.com. Accessed August 3, 2020.
Trygstad, T. (2019). Care Planning Is the Future of Pharmacy Practice. PharmacyTimes. https://www.pharmacytimes.com/publications/issue/2019/march2019/editors-note-care-planning-is-the-future-of-pharmacy-practice
Zellmer, W. A. (2012). The future of health-system pharmacy: opportunities and challenges in practice model change. Annals of Pharmacotherapy, 46(4_suppl), 41S-45S.