Pharmaceutical Care: Adherence Assessment and Medicines Related Problems (Part 2)
Pharmaceutical care, focused on medication adherence and addressing medicine-related problems, is crucial for improving patient outcomes.
Featured Blogger
August 17, 2025
11/11/23
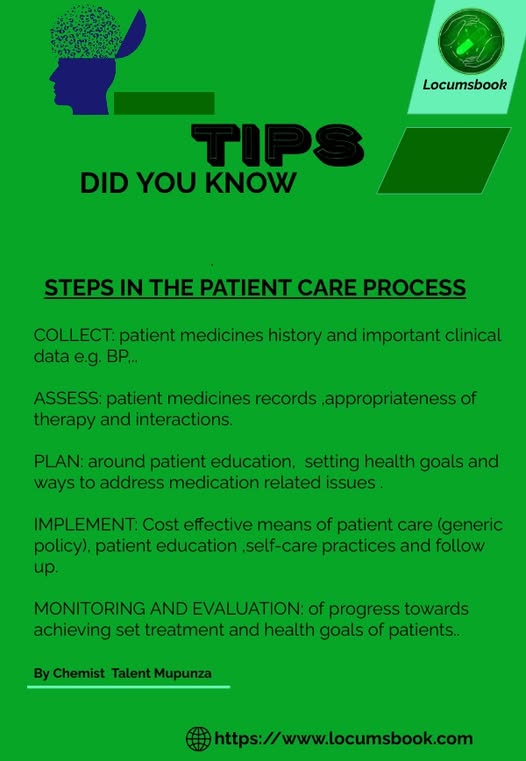
From the previous discussion we looked at the provision of pharmaceutical care and challenges involved in its implementation as well as some recommendations for improvement. This article seeks to reinforce the need optimal provision of pharmaceutical care by presenting some techniques to help patients manage drug therapy by building better patient understanding about their medication therapy and facilitating patient adherence to treatment regimens.
Background
Lack of patient adherence to medication therapy remains a major health issue according to a World Health Organization (2003) report.[1] As expected recent trends haven’t shown any significant improvement which is pretty much a common problem in our context.
Without putting special emphasis on the definition and methods of measurement, it is sure that adherence rates are well below 100%. The general consensus being that adherence rates for long-term therapies tend to be about 50%.[2][3] Numerous reasons exist for why adherence is less than optimal.
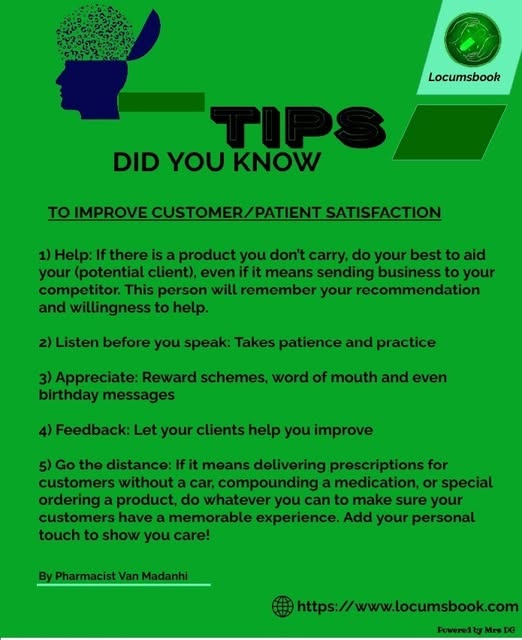
Some reasons are related to patients, some are related to health care providers, and others evolve from the health care delivery system. Before pharmacists are able to help a patient improve adherence to a treatment regimen, they must understand the underlying causes of the non-adherence in this particular patient. Non-adherence can be divided into two broad categories: unintentional or inadvertent non-adherence and intentional non-adherence.[4]
Inadvertent non-adherence typically involves forgetting to take medications at prescribed times. Intentional non-adherence involves decisions a patient has made to alter a medication regimen or to discontinue drug therapy (permanently or temporarily).
For example, a patient may decide to stop taking a medication due to an uncomfortable side effect or skip doses of a medication that should not be taken with alcohol before going to a party. It is important for a pharmacist not make generalized assumptions nor take for granted that patients understand all aspects of their drug therapy before they get to the pharmacy and as such pharmacists should not assume:
● that physicians have already discussed with patients the medications they prescribe,
● that patients understand all information provided. Even seemingly straightforward label directions like “take one tablet every six hours” are misinterpreted by a large percentage of patients (which may result in some patients taking less than required does as they interpret the 6 hourly interval as “during the day hours only-think of cloxacillin regimen”
● that when patients do not take their medications correctly that they “don’t care,” “aren’t motivated,” “lack intelligence,” or “can’t remember.” These assumptions prevent you from focusing on the real problems causing non-adherence.[4]
● that once patients start taking their medications correctly, they will continue to take them correctly in the future-I am of the opinion that pharmacists refrain from using the :”To be taken as before” label. Rather communicate and be sure the patient is taking the medication concordantly.
Techniques to Improve Patient Understanding
◾ Give reasons for key advice.
For example, with an antibiotic prescription, tell why it is necessary to continue medication use even though symptoms have disappeared. Patients should understand the reasons behind what you and the physician are instructing them. When reasons for advice are provided, patients are more likely to perceive the advice as important.
◾ Provide key information at the beginning and end of the interaction.
Patients concentrate on the initial information given and also remember the last items discussed.
◾ End the encounter by giving patients the opportunity to provide feedback about what they learned.
You should ask patients to summarize critical points of information so that you can make sure you communicated clearly and patients understand accurately. If patients do not understand, this is not a reflection on them but rather is an indication that you must do a better job in communication and educational efforts.
◾ Supplementing oral instructions with written information where necessary.
Refer to advice in the written information as you counsel patients. To be better explain, some packaging bags have pictographs to indicate times of the day, so pharmacists can take advantage of that by even adding info on to that e.g number of tablets. [4]
Medication-related problems (MRPs)
Here I do not wish to put any emphasis but just to highlight the fact that when the use of medicines is not optimum, we’re likely going to encounter MRPs.
As you have seen in the previous discussions the majority of these issues are eliminated the the optimal provision of pharmaceutical care (including but not limited to effective communication, enhancing adherence and influencing positive behavior in patients).
References:
1.Brown MT, Bussell JK. Medication adherence: WHO cares? [Internet]. Mayo Clinic proceedings. Mayo Foundation for Medical Education and Research; 2011 [cited 2020Oct17]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3068890/
2.Martin, L., Williams, S., Haskard, K., & Dimatteo, M. (2005, September). The challenge of patient adherence. Retrieved October 17, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1661624/
3.Brenda Wood, P. (2012, April 23). Medication Adherence: The Real Problem When Treating Chronic Conditions. Retrieved October 17, 2020, from https://www.uspharmacist.com/.../medication-adherence-the...
4.Tindall, W. N., Beardsley, R. S., & Kimberlin, C. L. (2008). Helping Patients Manage Therapeutic Regimens. In Communication skills in pharmacy practice a practical guide for students and practitioners. Philadelphia: Lea & Febiger.